Difficult Case Types, Part 1: A Discussion of Adult Short-Term Orthodontics
Originally posted on Dentistry Today.
INTRODUCTION
Short-term orthodontics (STO) has exploded in popularity during the past 10 years. Adults are discovering that they are able to straighten their anterior teeth cosmetically without undergoing 2 years of bite-changing orthodontics, and are enthusiastically seeking out this treatment.
Since I first wrote about “Adult 6-Month Orthodontics” in 1999 for Dentistry Today,1 Ryan Swain (Six Month Smiles) and other general dentists and some orthodontists, have been teaching STO in the United States, Europe, and Australia to enthusiastic audiences. There is good reason for this—orthodontists have not supported a strong case for routinely prescribing 2-year orthodontics with a Class I molar occlusion as its focus. Moreover, the evidence in the literature for the benefits of moving molars already in functional occlusion (except, for example, correction of a posterior edge-edge bite causing attrition) is underwhelming.
Adults do not generally seek orthodontic treatment and wear braces mainly for their molars, and 2-year treatment for profile change is not generally possible nonsurgically in the adult patient. When it is done, profile changes are difficult to retain. Although visits must be longer for STO and retention protocol more stringent, it is a great new service that is bringing many back to dentistry. As Dr. Gordon Christensen stated, “I feel certain that may more people would have orthodontic therapy if it could be simplified and made more acceptable to them as adults….I congratulate you for your innovative and thoughtful approach to the subject” (Dr. Gordon Christensen, personal correspondence in writing, January 4, 2000 and January 29, 2004). A general practice performing this treatment will experience a boon to its periodontic, endodontic, and restorative services, in addition to its bleaching and veneer offerings, as a healthy mouth precedes the healthy smile in treatment planning. This is truly a valuable service to the public.
Orthodontist Jack Sheridan2 pioneered interproximal reduction in the 1970s and promoted chief complaint orthodontics for years. His criteria was: (a) the occlusion is functional and the patient eats comfortably; (b) the patient’s chief complaint is crowded anterior teeth; (c) the crowding can be resolved without expansion and usually air-rotor stripping; (d) treatment time should be minimal, preferably about 6 months; (e) patients understand nighttime retainer wear may be permanent; and (f) patients understand that treatment is aesthetic only in nature (Dr. Jack Sheridan, personal correspondence in writing, June 5, 1997).
The cosmetic dentistry revolution has brought STO to the forefront, and it has become a field all its own. A wide array of problems can be dealt with in a different way when the focus is cosmetic. “Camouflage treatment” can be performed on Class III skeletal patients who decline orthognathic surgery by tipping mandibular incisors into a Class I incisor relation. Slight tipping of maxillary molars can be done in lieu of palatal surgery for the posterior edge to edge bite. Anterior crossbites can be corrected through lower incisor extractions if the patient’s profile is acceptable. As with many difficult cases, there often exist various solutions. With any new treatment approach, though, there also exist certain caveats, areas to watch out for, and pitfalls to avoid.
This article will be a review some of the most difficult cases I have seen during the past 20 years of performing STO on a wide variety of case types. Although there are traditional orthodontists and general dentists who would see this as an opportunity to categorically criticize STO, it is my hope instead that they seek to better understand the treatment, and to realize that it has a place in an array of cosmetic treatment options. Someday, they too may want to consider offering accelerated orthodontic treatment in adult cases that are strictly cosmetic, as it can be a superior and less invasive service than crowning or veneering crowded teeth. It should also be noted that many of the difficulties in the cases presented might have occurred with a longer treatment period.
CASE TYPE I: BRUXERS
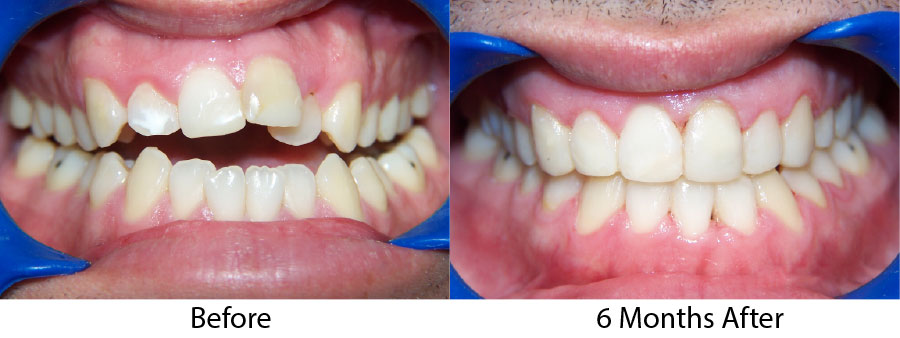
Severe bruxers who do not wear their nightguard often experience relapse after orthodontics. The patient in Figure 1 underwent STO for anterior space closure and achieved a nice aesthetic and occlusal result. However, retention for bruxers hinges on strict adherence to retainer wear as well as diligent nightguard use. As new abfractions are evident in the recall photo, he did not comply.
Throughout a period of 14 years post-treatment, the patient’s vertical dimension of occlusion (VDO) decreased. Two crowns were done to cover fluorosis. Although the protrusion and diastema did not significantly relapse, the deep bite returned (Figure 2). Though this may also occur in 2-year orthodontic cases, I more thoroughly emphasize strict adherence to nightguard use indefinitely in these cases. I inform bruxers that orthodontics is of minimal or no benefit if they are not prepared for a lifelong commitment to retention. Despite some relapse, he is still a satisfied patient in our practice 14 years later and fully understands the responsibility of retention lies with him through wearing his nightguard-Hawley combination at night.
 |
 |
| Figure 1. Preoperative: Before with diastema and deep bite from bruxing. |
Figure 2. Postoperative: The 14-year recall after 6-month short-term orthodontics (STO). The patient did not wear his nightguard. |
 |
 |
| Figure 3. Preoperative: Clencher before STO. |
Figure 4. Postoperative: Clencher, splinted. |
Similar to case 1, this patient was splinted and still experienced some relapse of her VDO at recall because of bruxism and limited nightguard wear. However, her alignment was maintained (Figures 3 and 4).
Figure 5 shows another patient who is a severe bruxer with flat plane occlusion. He experienced buccal migration of his upper first bicuspids post completion due to no nightguard wear. This occurred before postorthodontic settling took place, and articulating paper showed these bicuspids more heavily in occlusion than his molars. When he bruxed laterally, the buccal bone (which had not yet solidified) did not resist buccal tipping from the lateral forces on these teeth during parafunction.
Rarely is every tooth in complete occlusion postorthodontics, even with comprehensive treatment. Bruxers and clenchers usually experience more rapid post-treatment settling with more complete interdigitation than nonbruxers. But when the patient is a severe bruxer, selective migration may occur, especially if this is a flat plane occlusion with no cusps. This patient was rebracketed for 2 months before having a complete occlusion equilibration at the day of debracketing. Nightguard wear was strictly emphasized and the final result was stable.
CASE TYPE II: OBSESSIVE COMPULSIVE DISORDER TYPE COSMETIC PATIENTS
Another case type to watch for is the cosmetic patient who wants to dictate the treatment plan. While it is tempting to want to “please” a cosmetic patient, as it is an elective procedure after all, forging into a new area or performing a procedure with which you have less experience means less predictability in the final result. Doing this on patients who have exacting personalities and have a specific end result in mind further increases the risks involved. As with the bruxer category, patients like this can be red flags in cosmetic dentistry. These patients often start out with enthusiasm and seem to grasp the nuances of cosmetic dentistry, understanding the details of smile design. We may feel on the same page as these individuals who share our love for cosmetic excellence, and this makes dentistry fun. But when enthusiasm morphs into unrealistic expectations of perfection, and the patient cannot fully understand that there are limitations, difficulties may arise. Do we always know exactly what end result can and cannot be achieved? Are computer simulations really honest predictors of the end result, and should we depend on them to be accurate in every case? In a perfect world, we could predict all contingencies as well as the final result. But unless one has done every possible case type on every possible personality type with the various biologic limitations, there is no way anyone can predict the myriad of possibilities which may arise in every cosmetic case.
Case 1
This first case involves a simple level and alignment type orthodontic case with a slight open bite (Figure 6). Toward the end of treatment, though, the patient decided she also wanted anterior bonding to change her basic tooth shape from round to square. She brought in close-up photos of a famous American supermodel, and wanted her teeth to resemble this model’s smile. These teeth are square, slightly flared forward, and appear wider at the incisal than at the height of contour, usually the widest part of the tooth. When the patient presented for treatment, there was no indication her preferences were so specific. At this point in treatment, we are “married” to our patient, and separation is unfulfilling for both patient and dentist. After treatment, retention and incisal bonding were combined with a composite-Ribbond splint (Figure 7).3
 |
 |
Figure 5. Preoperative: Bruxer with flat plane
occlusion. |
Figure 6. Preoperative: STO with open bite. |
 |
 |
| Figure 7. Postoperative (after STO): Patient requested long square teeth like a famous supermodel she admired. |
Figure 8. Preoperative (before STO): Patient recently completed Invisalign treatment in another office. |
 |
 |
| Figure 9. Postoperative to short-term lingual orthodontics with custom requests. Patient wanted his centrals to be longer and a bit more protrusive and brought in a photograph of a famous actor’s teeth to copy. |
Figure 10. Preoperative: before STO. |
The splint helps to support more durable lengthening of the incisal edges, often done with porcelain veneers. While the orthodontics went smoothly, the final step of aesthetic bonding and recontouring was tedious and difficult.
Case 2
This patient had not long before completed Invisalign treatment elsewhere with acceptable results, but had very specific requests and a particular mental picture of how he wanted his teeth aligned and shaped. I was hesitant to take the case, as his alignment was already fairly good (Figure 8). A chief complaint list was made at the initial consult and twice reviewed with the patient. He chose lingual braces, the most difficult to control. He was advised that we may need to do some finishing with labial brackets in the final weeks. During treatment, his requests grew even more specific and he brought numerous hand-drawn sketches and a picture of a famous American actor’s smile to copy. More frequent visits were required, but the teeth were aligned in 4 months to his specifications, like this actor’s smile, with the upper centrals slightly protruding and longer (Figure 9). The patient completed treatment very happy with the result, but it is still risky to accept this case type knowing the patient has such a specific result in mind.
Case 3
This patient had become addicted to cosmetic surgery at a young age. At the consult, he expressed his dissatisfaction with his plastic surgeon despite what seemed were good results. Because his occlusion, crowding, and tooth morphology were so unaesthetic, it seemed that significant aesthetic improvement would not be difficult (Figure 10). However, the patient had numerous specific demands, including exact measurements for the lateral incisor veneers done after Figure 11. The final results were excellent but, again, the process difficult due to specific requests.
 |
 |
| Figure 11. After STO, but before porcelain veneers on teeth Nos. 7 and 10. |
Figure 12. The patient had central incisors extracted at a young age, before conventional 2-year orthodontics. |
 |
 |
| Figure 13. After distalizing lateral incisors. |
Figure 14. After retreatment with laterals brought back to mesial and 4 splinted crowns. |
CASE TYPE III: PATIENT ALTERS TREATMENT PLAN
To what extent do we try to please the patient? Figure 12 shows a patient who had orthodontics at age 13 years. Due to protrusive maxillary central incisors, the orthodontist decided to extract them and move laterals into the centrals’ position. With relapse, the spacing and recession is highly conspicuous. A simple treatment plan was given to consolidate the space through space closure and to provide 4 splinted crowns. When treatment began, however, the patient decided he wanted to re-establish the space for the missing central incisors to have a natural complement of teeth. As this was a patient in his 40s, the bone was not malleable. When space was established and a temporary bridge placed (Figure 13), there was slight overjet. Although I have before left overjet to provide space for a maxillary lingual splint without patient objection, this particular patient was not comfortable with his new incisor position forward. He felt that his maxillary incisal edges were noticeable, at times touching on his lower lip, although there was no deep bite. I referred him to a board-certified prosthodontist who felt there was nothing wrong with the bridge and that he could not improve significantly on the result. After a hiatus, the decision was made to retreat the case (at no change) and follow the original plan; consolidate the incisor space, and place splinted crowns. The end result satisfied the patient, and was more aesthetic, but the circuitous route there was difficult and spanned 4.5 years (Figure 14).
Bruxers, patients with obsessive compulsive disorder, and patients who alter their treatment plan represent challenging cases even when one is prepared for them and has treated similar cases previously. This is because no 2 orthodontic cases are ever identical when one considers the complete aesthetic, biologic, and interpersonal picture. We can only diligently try to consider all contingencies.
CLOSING COMMENTS
Treating such a variety of cases makes aesthetic orthodontics fascinating. Specialty orthodontic training often has a different focus which does not always encompass the adjunctive cosmetic dimension and adult psychological aspect central to success in some of these adult cosmetic cases. Furthermore, patients do not always afford us the 2 years of treatment time often needed to cross-refer across specialties and follow the traditional channels from decades past. As we listen more to our patients, the future of adult orthodontics is finally evolving, becoming a distinct area and more integrated with cosmetic dentistry.
In part 2 of this article, I will discuss transfer cases, improper use of enamel reproximation, cases with special retention needs, temporomandibular disorder sequelae, large tongues, problem profiles, and multidisciplinary cases that have unique challenges which fall out of the norm of traditional orthodontic cases.
References
- Georgaklis CC. Six-month adult aesthetic orthodontic treatment. Dent Today. 1999;18:110-113.
- Sheridan JJ, Ledoux PM. Air-rotor stripping and proximal sealants. An SEM evaluation. J Clin Orthod. 1989;23:790-794.
- Georgaklis CC. Anterior retention with a reinforced composite resin splint after cosmetic orthodontic treatment.
- ‘;. 2002;21:54-57.